Painless death has become an increasingly important topic in modern discussions about end-of-life care and medical ethics. As society continues to evolve, so too does our understanding of what it means to die with dignity and without suffering. In this article, we will explore the concept of painless death, its significance, and the various factors that contribute to achieving such an outcome.
End-of-life care is a sensitive subject that affects everyone, regardless of age or health status. Understanding the principles behind painless death can help individuals and families make informed decisions about their care options. This knowledge empowers them to navigate the complex landscape of medical treatments and palliative care services.
In this comprehensive guide, we will delve into the intricacies of painless death, including its definition, methods, ethical considerations, and the role of modern medicine in facilitating a peaceful transition. By the end of this article, you will have a clearer understanding of how to approach this topic with confidence and compassion.
Table of Contents:
- What is Painless Death?
- Methods of Achieving Painless Death
- Ethical Considerations
- Role of Modern Medicine
- End-of-Life Care Options
- Legal Frameworks
- Palliative Care
- Psychological and Emotional Support
- Frequently Asked Questions
- Conclusion
What is Painless Death?
Painless death refers to the process of dying without experiencing significant physical or emotional suffering. It emphasizes the importance of dignity, comfort, and compassion during the final stages of life. Achieving a painless death requires a multidisciplinary approach that involves medical professionals, caregivers, and family members working together to ensure the best possible outcome for the individual.
The concept of painless death is closely tied to the principles of palliative care, which focuses on relieving symptoms and improving quality of life for patients with serious illnesses. By addressing both physical and emotional needs, palliative care aims to provide a holistic approach to end-of-life care that prioritizes the well-being of the patient.
Key Components of Painless Death
- Pain Management: Effective pain management is essential for ensuring a peaceful transition. This may involve the use of medications, therapies, or other interventions tailored to the individual's needs.
- Emotional Support: Providing emotional support to both the patient and their loved ones can help alleviate anxiety and stress during this challenging time.
- Communication: Open and honest communication between healthcare providers, patients, and families is crucial for making informed decisions about care options.
Methods of Achieving Painless Death
There are several methods and approaches that can contribute to achieving a painless death. These methods vary depending on the individual's medical condition, personal preferences, and cultural beliefs. Below, we will explore some of the most common techniques used in modern end-of-life care.
1. Palliative Sedation
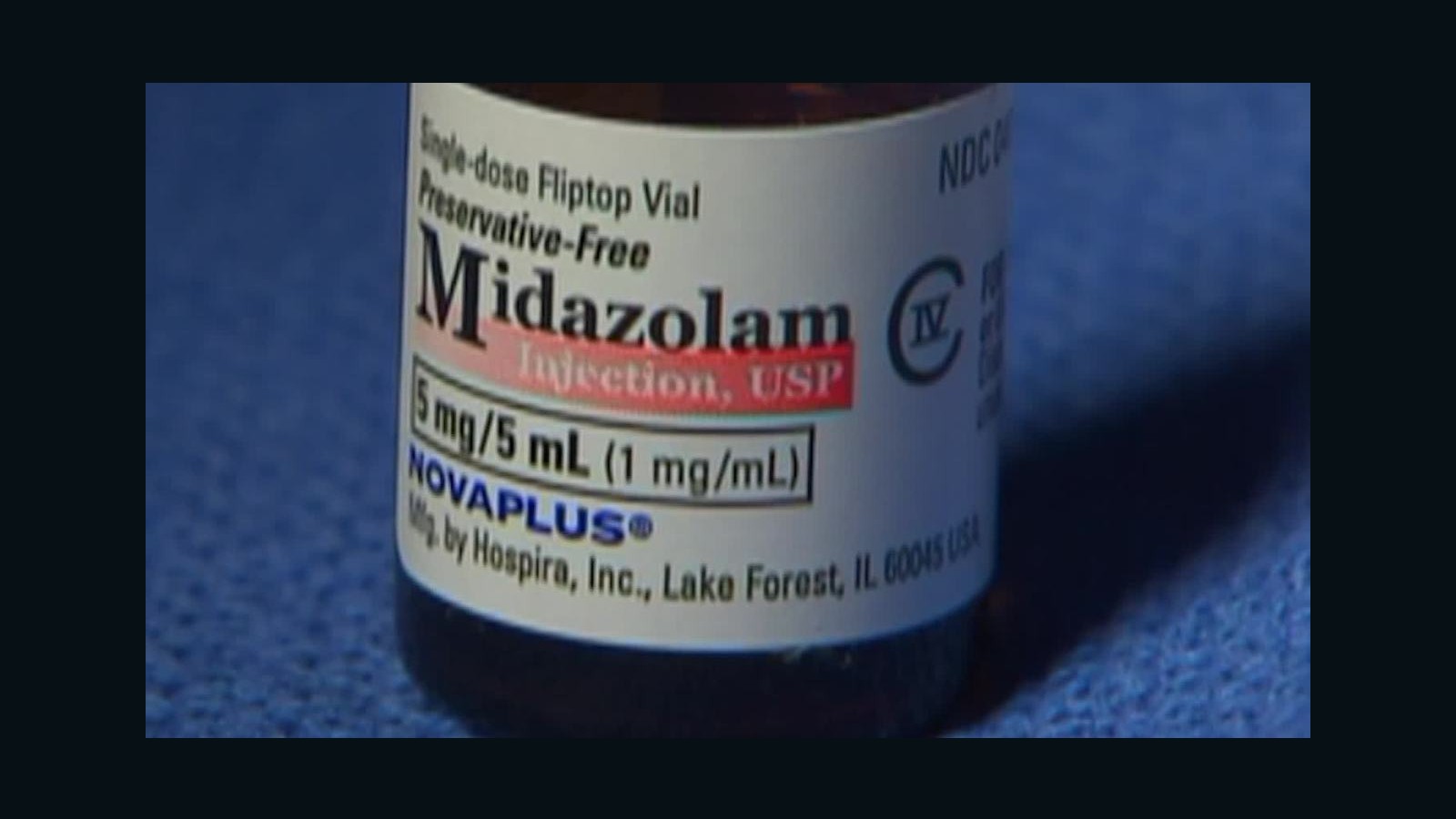
Palliative sedation involves the use of medications to induce a state of unconsciousness in patients experiencing severe and intractable suffering. This approach is typically reserved for cases where other pain management strategies have proven ineffective. According to the World Health Organization (WHO), palliative sedation should be used as a last resort when all other options have been exhausted.
2. Hospice Care
Hospice care is a specialized form of palliative care that focuses on providing comfort and support to terminally ill patients and their families. Hospice services are typically provided in a home setting or in a dedicated hospice facility, allowing patients to spend their final days in a familiar and supportive environment.
Ethical Considerations
The pursuit of painless death raises several ethical questions that must be carefully considered by healthcare providers, policymakers, and society as a whole. These questions often revolve around issues of autonomy, beneficence, and justice, as well as the potential for abuse or misuse of certain practices.
1. Patient Autonomy
Respecting the autonomy of patients is a fundamental principle in medical ethics. This means allowing individuals to make informed decisions about their care, including the option to pursue painless death if they so choose. However, ensuring that patients are fully informed and capable of making such decisions can be challenging, particularly in cases where cognitive impairment or other factors may be present.
2. Slippery Slope Argument
Some critics argue that legalizing or promoting painless death could lead to a "slippery slope," where vulnerable populations may feel pressured to choose euthanasia or other forms of assisted death to avoid being a burden on their families or society. Addressing these concerns requires careful consideration of legal safeguards and ethical guidelines.
Role of Modern Medicine
Modern medicine plays a crucial role in facilitating painless death through advancements in pain management, palliative care, and end-of-life interventions. These developments have significantly improved the quality of care available to patients and their families, enabling more people to experience a peaceful and dignified passing.
Research published in the Journal of Pain and Symptom Management highlights the importance of interdisciplinary collaboration in providing comprehensive end-of-life care. By combining the expertise of physicians, nurses, social workers, and other professionals, healthcare teams can develop personalized care plans that address the unique needs of each patient.
End-of-Life Care Options
Individuals and families facing end-of-life decisions have several care options to consider, each with its own benefits and limitations. Understanding these options can help them make informed choices that align with their values and preferences.
1. Home Care
Many people prefer to spend their final days at home, surrounded by loved ones and familiar surroundings. Home care services can provide the necessary support to make this possible, including nursing care, medication management, and emotional support for family members.
2. Inpatient Hospice
Inpatient hospice facilities offer a more structured environment for patients requiring intensive care or support. These facilities are staffed by experienced professionals who specialize in end-of-life care, ensuring that patients receive the highest level of comfort and dignity.
Legal Frameworks
The legal landscape surrounding painless death varies significantly across different countries and jurisdictions. In some places, assisted death is legally permitted under certain conditions, while in others, it remains strictly prohibited. Understanding the legal implications of painless death is essential for both healthcare providers and patients.
For example, in countries like Canada and the Netherlands, assisted death is legal under specific circumstances, such as terminal illness or unbearable suffering. In contrast, many other countries have yet to adopt similar legislation, leaving patients and families to navigate complex ethical and legal challenges.
Palliative Care
Palliative care is a critical component of painless death, focusing on relieving symptoms and improving quality of life for patients with serious illnesses. This approach emphasizes a patient-centered model of care that addresses both physical and emotional needs, ensuring that individuals receive the support they need during their final days.
According to the National Institutes of Health (NIH), early integration of palliative care into the treatment plan can lead to improved outcomes for patients and their families. This includes better symptom management, increased satisfaction with care, and reduced healthcare costs.
Psychological and Emotional Support
Providing psychological and emotional support is an essential aspect of achieving a painless death. This support can take many forms, including counseling, spiritual guidance, and peer support groups. By addressing the emotional needs of both patients and their loved ones, caregivers can help alleviate anxiety and stress during this difficult time.
1. Counseling Services
Counseling services can help patients and families process their emotions and come to terms with the impending loss. These services may be provided by licensed therapists, social workers, or other trained professionals, depending on the individual's needs and preferences.
2. Spiritual Guidance
For many people, spiritual guidance plays an important role in coping with end-of-life issues. Clergy members, chaplains, or other spiritual advisors can offer comfort and support during this challenging time, helping individuals find meaning and purpose in their final days.
Frequently Asked Questions
Here are some common questions and answers about painless death:
- Q: Is painless death the same as euthanasia? A: While both involve efforts to reduce suffering, painless death encompasses a broader range of approaches, including palliative care and hospice services, whereas euthanasia specifically refers to the intentional ending of life.
- Q: Are there any risks associated with painless death? A: As with any medical intervention, there are potential risks and side effects associated with painless death. However, these risks can often be minimized through careful planning and collaboration with healthcare professionals.
Conclusion
Painless death represents a compassionate and dignified approach to end-of-life care that prioritizes the well-being of patients and their families. By understanding the principles and methods involved in achieving a painless death, individuals can make informed decisions about their care options and ensure a peaceful transition.
We invite you to share your thoughts and experiences in the comments section below. Additionally, feel free to explore other articles on our site for more information on related topics. Together, we can promote greater awareness and understanding of the importance of painless death in modern healthcare.